
Water Quality
Safe drinking water is essential for our bodies to function properly, supporting vital processes such as digestion, circulation, temperature regulation, and overall health. Staying hydrated with clean, safe water helps maintain energy levels, enhances focus, and enables us to perform at our best both physically and mentally. Without access to quality drinking water, our ability to thrive and achieve our full potential can be at risk.
At Advantage Environmental, our team has the experience and understanding to ensure the accuracy of each result. Our team can test lead, copper, total coliform/E. coli, Legionella, Chlorine, PH, for water outlets primarily designed for human consumption. AEI will also check the levels for PH, Chlorine, and temperature to help diagnose the efficiency and performance of the treatment system. With established guidelines, AEI is committed to supporting the mission of achieving and maintaining compliance.
GSA Water Testing
The General Services Administration’s (GSA) Order on Drinking Water Quality Management has been a foundational policy for ensuring high drinking water standards within the U.S. General Services Administration’s Public Building Service (PBS). Beginning in 2024, all active and occupied federally owned facilities exceeding 1,000 square feet and equipped with drinking water systems have undergone initial water quality testing. All GSA owned or leased properties will be tested for lead in water, copper in water, total coliform/E. coli, and legionella, per the GSA Order for Drinking Water Quality Management (PBS 1000.7A). Additionally, starting February 2024, the GSA issued change orders to approximately 6,400 existing lease contracts, mandating one-time drinking water testing. Nationwide, the GSA manages 1,410 owned facilities and leases 5,979 properties, per the GSA website.

Why is baseline testing for water quality important?
Baseline testing establishes the current condition of a water system, serving as a reference for identifying future changes or issues. By identifying contaminants or bacteria, such as Legionella, building managers can implement appropriate control measures to maintain safe drinking water.
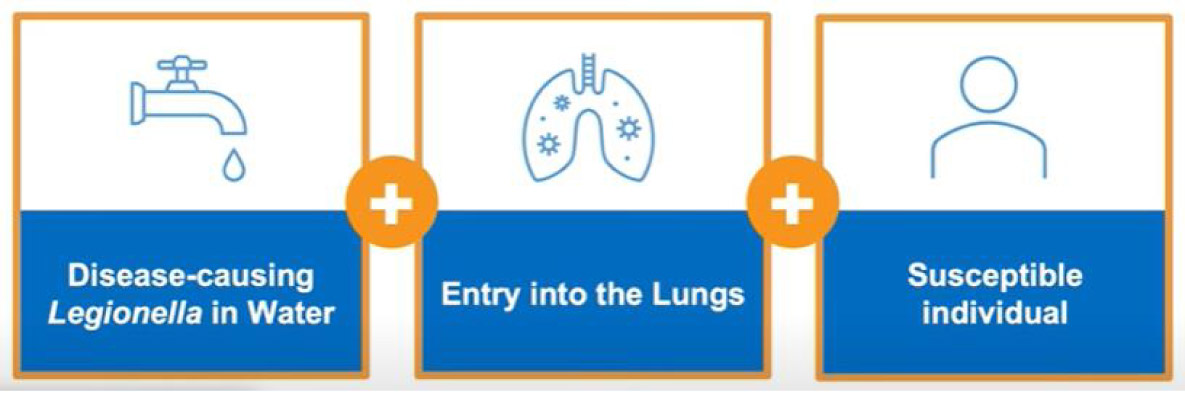
What is Legionella and the related risk?
Legionella bacteria can occur in freshwater environments and water systems in built environments. Legionella grows well in warm water and can multiply in large or complex water systems, like those found in office buildings. Common sources of exposure also include schools, hotels, grocery stores, and our homes.
• High Risk (cooling towers, decorative fountains, hot tubs, and humidifiers)
• Medium Risk (showers)
• Low Risk (sinks, water fountains, and other fixtures used for drinking or washing).
People can become ill with Legionnaires’ disease (LD) or Pontiac fever (PF) when they inhale aerosolized water containing Legionella. Legionella exposure primarily occurs through inhalation rather than ingestion. While certain high-risk populations may experience different exposure routes, inhalation remains the primary route. Legionnaires disease does not normally spread from person to person. According to the CDC, the risk of getting sick from a building’s water supply is exceptionally low, especially for healthy people including children. People at increased risk of getting sick are:
• People with a chronic lung disease (like chronic obstructive pulmonary disease or emphysema)
• People with weak immune systems or who take drugs that weaken the immune system (like after a transplant operation or chemotherapy)
• People 50 years or older (especially if you smoke cigarettes).
The Centers for Disease Control and Prevention (CDC) has tracked cases of Legionnaires Disease since the 1990’s. From 2000-2018, the number of cases has increased 9-fold.
Lead and Copper in Drinking Water
Lead and copper in drinking water have been topics of concern for public health due to their potential adverse effects on human health, particularly in high concentrations. In older homes and buildings, lead can leach from service lines, solder, and fixtures into tap water and become a significant source of lead exposure. In children, lead exposure can cause irreversible and life-long health effects, including decreasing IQ, focus, and academic achievement. On December 22, 2020, U.S. Environmental Protection Agency (EPA) finalized the first major update to the Lead and Copper Rule (LCR) in nearly 30 years. EPA’s new rule uses science-based testing protocols to find more sources of lead in drinking water.
• Lead can enter drinking water primarily through corrosion of lead-containing plumbing materials, such as pipes, fittings, and fixtures. Older homes, built prior to the 1980s, are more likely to have lead plumbing.
• Even low levels of lead exposure can have harmful effects, especially in children. It can affect the nervous system, kidney function, and blood cells. Pregnant women are also at risk because lead can pass from the mother to the fetus.
• Copper contamination in drinking water often results from corrosion of copper pipes and fittings. Like lead, older homes with copper plumbing systems are more likely to have higher copper levels in their water.
• While copper is an essential nutrient at low levels, high concentrations can cause health problems such as gastrointestinal issues, liver and kidney damage, and Wilson's disease in individuals with a genetic predisposition.
Total Coliform/E. Coli in Drinking Water
Testing drinking water for all possible pathogens is complex, time-consuming, and expensive. It is relatively easy and inexpensive to test for coliform bacteria. There are three groups of coliform bacteria; each has a different level of risk.
• Total coliform bacteria encompass nineteen genera commonly found in the environment, including soil, decaying vegetation, plants, and the gastrointestinal tract of warm-blooded animals. Their presence in water signals potential contamination from various environmental sources or fecal matter.
• Fecal coliform bacteria are a sub-group of coliform or TC that appears in copious quantities in people and animals. The presence of fecal coliform in drinking water often indicates that there has been fecal contamination in the water. Fecal coliform is also referred to as “thermotolerant coliforms” as they can thrive around 111.2 °F (44°C)
• Escherichia coli (E. Coli) bacteria are found in the large intestine or feces of healthy warm-blooded animals and humans. Most E. coli strains are harmless and serve a useful function in the body by stopping the growth of harmful bacteria species and by making necessary vitamins, per the Safe Drinking Water Foundation website. Most forms of E. Coli can cause brief diarrhea.
• E. Coli 0157:H7 is a rare, specific strain of E. Coli that can produce a powerful toxin that damages the lining of the small intestine. Causing health effects like a bloody stool, stomach pain, nausea and vomiting in some people, according to the Mayo Clinic website.
There are certain risk factors that could increase the chance of infection or getting seriously ill, according to the Center of Disease Control (CDC). These groups include:
• Children who are younger than 5 years old
• Adults who are 65 years old and older
• People who have a weakened immune system

Private Well Water Testing
If you own a private well, you are responsible for testing your own water. In most counties when you buy or sell a home with a private well, the county health or planning department, or the lending institution involved, may require the seller to provide water-sampling results to show the water is safe to drink. Contact your local county health or planning department for information on the requirements and the testing needed.
Department of Health (DOH) recommends that private well owners test their drinking water every year for coliform bacteria and nitrate. These two contaminants rapidly could affect a person's health—possibly even with just one drink of water. If your nitrate level is 5 milligrams per liter (mg/L) or higher, you may want to re-test in six months.
At least twice, while you own the well, we also suggest testing for arsenic – once in summer and again in winter – to check any seasonal influences that may occur. Though arsenic does not cause rapid health effects, continued consumption over a relatively short time could lead to health concerns. Many certified labs in Washington perform these tests.
Other contaminants
If you have a concern about other contaminants, you can get your well water tested, including:
• Chromium
• Copper
• Cryptosporidium
• Disinfection byproducts
• Lead
• Manganese
• Per- and polyfluoroalkyl substances (PFAs)
Coliform Bacteria
Test for coliform bacteria at least once a year, or when...
• A household member has an unexplained illness
• You hear your neighbor's well is contaminated or they have a failing septic system
• You notice a change in your water's appearance, taste, or smell
• You replace or repair any part of your well system
• Your well has been flooded
Testing your water for coliform bacteria can alert you to fecal pollution that may be contaminating your well. Fecal pollution can come from various sources, such as a failing septic system or livestock manure nearby. Fecal coliform bacteria can cause illness in humans.
Nitrates
Test for nitrates at least once a year, or when...
• A household member is an infant under 12 months old
• A household member is pregnant, nursing, or trying to get pregnant
• You live in an area where fertilizers are, or have been, used near your well
Exposure to nitrates above the recommended level can cause illness and death in infants below the age of six months. Symptoms include shortness of breath and blue-baby syndrome. Nitrates can come from fertilizer runoff, leaking septic tanks/sewage, or erosion of natural deposits.
Arsenic
Because the amount of arsenic in well water can vary throughout the year, test for arsenic once in the late summer and once again in the early spring to see if there are seasonal differences. You may also want to test if:
• You live in an area known to have naturally occurring arsenic in the groundwater
• You know of neighbors who have high arsenic in their wells
Long term exposure to even small amounts of arsenic can increase the risk of developing certain health conditions such as cancer, while consuming high levels of arsenic can cause immediate and severe health effects as well.
A note about arsenic: When wells are accepted as a source of drinking water, the water must be tested for arsenic among other contaminants. Well water that tests high must have an approved treatment system installed before being accepted as a drinking water supply, and an arsenic disclosure form must be recorded onto the property title. However because arsenic levels can vary, a well drilled years ago may not have had arsenic at the time, but it could now. This is another reason to test your well water regularly.
AAMI ST108 Critical Water
AAMI ST108 in healthcare facilities should: conduct a thorough audit of their existing water treatment systems, train staff on the standard's requirements, establish a robust monitoring program, regularly test water quality, and update policies and procedures to align with the new standard, potentially requiring upgrades to water treatment infrastructure to meet the necessary water quality levels for medical device reprocessing; involving a multidisciplinary team including engineering, infection control, and sterile processing personnel is crucial for successful implementation.
The standard is important for patient safety and equipment integrity. It ensures that water used to clean, disinfect, rinse, and sterilize medical devices is of adequate quality
• Water Quality Assessment:
• Analyze existing tap water quality through accredited laboratories to determine if additional treatment is needed.
• Identify different water quality categories (e.g., utility, critical) required for different stages of medical device processing.
• System Evaluation and Upgrades:
• Audit existing water treatment systems to assess their capability to meet ST108 standards.
• Consider necessary upgrades or installations of new water treatment systems like reverse osmosis units to achieve required water purity.
• Staff Training:
• Educate all relevant personnel, including sterile processing staff, on the AAMI ST108 standard, its importance, and their roles in maintaining water quality.
• Provide training on proper sampling techniques, monitoring procedures, and interpreting test results.
• Monitoring and Testing:
• Establish a comprehensive water quality monitoring plan with regular testing at designated sampling points.
• Monitor key parameters like conductivity, pH, microbial counts, and endotoxin levels according to the standard.
• Utilize validated testing methods and accredited laboratories.
• Policy and Procedure Updates:
• Review and revise existing water management plans to align with AAMI ST108 requirements.
• Document procedures for water treatment, monitoring, corrective actions, and reporting.
• Compliance and Quality Assurance:
• Establish a system to track and document compliance with AAMI ST108 standards.
• Conduct regular audits to identify potential issues and ensure ongoing compliance.
